Zika virus (ZIKV) is a member of the virus family Flaviviridae.[3] It is spread by daytime-active Aedes mosquitoes, such as A. aegypti and A. albopictus.[3] Its name comes from the Ziika Forest of Uganda, where the virus was first isolated in 1947.[4]Zika virus is related to the dengue, yellow fever, Japanese encephalitis, and West Nile viruses.[4] Since the 1950s, it has been known to occur within a narrow equatorial belt from Africa to Asia. From 2007 to 2016, the virus spread eastward,across the Pacific Ocean to the Americas, leading to the 2015–16 Zika virus epidemic.[5]
The infection, known as Zika fever or Zika virus disease, often causes no or only mild symptoms, similar to a very mild form ofdengue fever.[3] While there is no specific treatment, paracetamol (acetaminophen) and rest may help with the symptoms.[6]As of 2016, the illness cannot be prevented by medications or vaccines.[6] Zika can spread from a pregnant woman to her baby. This can result in microcephaly, severe brain malformations, and other birth defects.[7][8] Zika infections in adults may result rarely in Guillain–Barré syndrome.[9]
In January 2016, the United States Centers for Disease Control and Prevention (CDC) issued travel guidance on affected countries, including the use of enhanced precautions, and guidelines for pregnant women including considering postponing travel.[10][11] Other governments or health agencies also issued similar travel warnings,[12][13][14] while Colombia, theDominican Republic, Puerto Rico, Ecuador, El Salvador, and Jamaica advised women to postpone getting pregnant until more is known about the risks.[13][15] Zika is pronounced /ˈziːkə/ or /ˈzɪkə/.[16][17The Zika virus belongs to the Flaviviridae family and the Flavivirus genus, and is thus related to the dengue, yellow fever, Japanese encephalitis, and West Nileviruses. Like other flaviviruses, Zika virus is enveloped and icosahedral and has a nonsegmented, single-stranded, 10 kilobase positive-sense RNA genome. It is most closely related to the Spondweni virus and is one of the two known viruses in the Spondweni virus clade.[18][19][20][21][22]
A positive-sense RNA genome can be directly translated into viral proteins. As in other flaviviruses, such as the similarly sized West Nile virus, the RNA genome encodes seven nonstructural proteins and three structural proteins.[24] One of the structural proteins encapsulates the virus. This protein is the flavivirus envelope glycoprotein, that binds to the endosomal membrane of the host cell to initiate endocytosis.[25] The RNA genome forms a nucleocapsid along with copies of the 12-kDa capsid protein. The nucleocapsid, in turn, is enveloped within a host-derived membrane modified with two viral glycoproteins. Viral genome replication depends on the making of double stranded RNA from the single stranded positive sense RNA (ssRNA(+)) genome followed by transcription and replication to provide viral mRNAs and new ssRNA(+) genomes.[26][27]
There are two Zika lineages: the African lineage and the Asian lineage.[28] Phylogenetic studies indicate that the virus spreading in the Americas is 89% identical to African genotypes, but is most closely related to the Asian strain that circulated in French Polynesia during the 2013–2014 outbreak.[28][29][30]
The Asian strain appears to have evolved about 1939.[31]
Transmission[edit]
The vertebrate hosts of the virus were primarily monkeys in a so-called enzootic mosquito-monkey-mosquito cycle, with only occasional transmission to humans. Before the current pandemic began in 2007, Zika "rarely caused recognized 'spillover' infections in humans, even in highly enzootic areas". Infrequently, however, other arboviruses have become established as a human disease and spread in a mosquito–human–mosquito cycle, like the yellow fever virus and the dengue fever virus (both flaviviruses), and the chikungunya virus (a togavirus).[32] Though the reason for the pandemic is unknown, dengue, a related arbovirus that infects the same species of mosquito vectors, is known in particular to be intensified by urbanizationand globalization.[33] Zika is primarily spread by Aedes aegypti mosquitoes,[34] and can also be transmitted through sexual contact[35] or blood transfusions.[36] The basic reproduction number (R0, a measure of transmissibility) of Zika virus has been estimated to be between 1.4 and 6.6.[37]
In 2015, news reports drew attention to the rapid spread of Zika in Latin America and the Caribbean.[38] At that time, the Pan American Health Organizationpublished a list of countries and territories that experienced "local Zika virus transmission" comprising Barbados, Bolivia, Brazil, Colombia, the Dominican Republic, Ecuador, El Salvador, French Guiana, Guadeloupe, Guatemala, Guyana, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Puerto Rico, Saint Martin, Suriname, and Venezuela.[39][40][41] By August 2016, more than 50 countries had experienced active (local) transmission of Zika virus.[42]
Mosquito[edit]
Zika is primarily spread by the female Aedes aegypti mosquito, which is active mostly in the daytime.[43][44]The mosquitos must feed on blood in order to lay eggs.[45]:2 The virus has also been isolated from a number of arboreal mosquito species in the Aedes genus, such as A. africanus, A. apicoargenteus, A. furcifer, A. hensilli, A. luteocephalus and A. vittatus, with an extrinsic incubation period in mosquitoes of about 10 days.[21]
The true extent of the vectors is still unknown. Zika has been detected in many more species of Aedes, along with Anopheles coustani, Mansonia uniformis, and Culex perfuscus, although this alone does not incriminate them as a vector.[44]
Transmission by A. albopictus, the tiger mosquito, was reported from a 2007 urban outbreak in Gabon where it had newly invaded the country and become the primary vector for the concomitant chikungunyaand dengue virus outbreaks.[46] There is concern for autochthonous infections in urban areas of European countries infested by A. albopictus because the first two cases of laboratory-confirmed Zika infections imported into Italy were reported from viremic travelers returning from French Polynesia.[47]
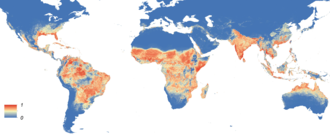
The potential societal risk of Zika can be delimited by the distribution of the mosquito species that transmit it. The global distribution of the most cited carrier of Zika,A. aegypti, is expanding due to global trade and travel.[48] A. aegypti distribution is now the most extensive ever recorded – across all continents including North America and even the European periphery (Madeira, the Netherlands, and the northeastern Black Sea coast).[49] A mosquito population capable of carrying Zika has been found in a Capitol Hill neighborhood of Washington, D. C., and genetic evidence suggests they survived at least four consecutive winters in the region. The study authors conclude that mosquitos are adapting for persistence in a northern climate.[50] The Zika virus appears to be contagious via mosquitoes for around a week after infection. The virus is thought to be infectious for a longer period of time after infection (at least 2 weeks) when transmitted via semen.[51][52]
Research into its ecological niche suggests that Zika may be influenced to a greater degree by changes in precipitation and temperature than Dengue, making it more likely to be confined to tropical areas. However, rising global temperatures would allow for the disease vector to expand their range further north, allowing Zika to follow.[53]
Sexual[edit]
Zika can be transmitted from men and women to their sexual partners; most known cases involve transmission from symptomatic men to women.[54][35][55] As of April 2016, sexual transmission of Zika has been documented in six countries – Argentina, Chile, France, Italy, New Zealand, and the United States – during the 2015 outbreak.[9]
Since October 2016, the CDC has advised men who have traveled to an area with Zika should use condoms or not have sex for at least six months after their return as the virus is still transmissible even if symptoms never develop.[56]
Pregnancy[edit]
The Zika virus can spread by vertical (or "mother-to-child") transmission, during pregnancy or at delivery.[57][7]
Blood transfusion[edit]
As of April 2016, two cases of Zika transmission through blood transfusions have been reported globally, both from Brazil,[36] after which the US Food and Drug Administration (FDA) recommended screening blood donors and deferring high-risk donors for 4 weeks.[58][59] A potential risk had been suspected based on a blood-donor screening study during the French Polynesian Zika outbreak, in which 2.8% (42) of donors from November 2013 and February 2014 tested positive for Zika RNA and were all asymptomatic at the time of blood donation. Eleven of the positive donors reported symptoms of Zika fever after their donation, but only three of 34 samples grew in culture.[60]
Pathogenesis[edit]
Zika virus replicates in the mosquito's midgut epithelial cells and then its salivary gland cells. After 5–10 days, the virus can be found in the mosquito’s saliva. If the mosquito’s saliva is inoculated into human skin, the virus can infect epidermal keratinocytes, skin fibroblasts in the skin and the Langerhans cells. The pathogenesis of the virus is hypothesized to continue with a spread to lymph nodes and the bloodstream.[18][61] Flaviviruses replicate in the cytoplasm, but Zika antigens have been found in infected cell nuclei.[62]
Zika fever[edit]
Zika fever (also known as Zika virus disease) is an illness caused by the Zika virus.[63] Most cases have no symptoms, but when present they are usually mild and can resemble dengue fever.[63][64] Symptoms may include fever, red eyes, joint pain, headache, and a maculopapular rash.[63][65][66] Symptoms generally last less than seven days.[65] It has not caused any reported deaths during the initial infection.[64] Infection during pregnancy causes microcephaly and other brain malformations in some babies.[7][8] Infection in adults has been linked to Guillain–Barré syndrome (GBS).[64]
Diagnosis is by testing the blood, urine, or saliva for the presence of Zika virus RNA when the person is sick.[63][65]
Prevention involves decreasing mosquito bites in areas where the disease occurs, and proper use of condoms.[65][67] Efforts to prevent bites include the use of insect repellent, covering much of the body with clothing, mosquito nets, and getting rid of standing water where mosquitoes reproduce.[63] There is no effective vaccine.[65] Health officials recommended that women in areas affected by the 2015–16 Zika outbreak consider putting off pregnancy and that pregnant women not travel to these areas.[65][68] While there is no specific treatment, paracetamol (acetaminophen) and rest may help with the symptoms.[65]Admission to hospital is rarely necessary.[64]
Vaccine development[edit]
The World Health Organization (WHO) has suggested that priority should be to develop inactivated vaccines and other non-live vaccines, which are safe to use in pregnant women.[69]
As of March 2016, 18 companies and institutions were developing vaccines against Zika but they state a vaccine is unlikely to be widely available for about ten years.[69][70]
In June 2016 the FDA granted the first approval for a human clinical trial for a Zika vaccine.[71] In March 2017, a DNA vaccine was approved for phase 2 clinical trials. This vaccine consists of a small circular piece of DNA, known as a plasmid, that expresses the genes for the Zika virus envelope proteins. As the vaccine does not contain the full sequence of the virus, it cannot cause infection.[72] As of April 2017, both subunit and inactivated vaccines have entered clinical trials.[73]
History[edit]
Virus isolation in monkeys and mosquitoes, 1947[edit]
The virus was first isolated in April 1947 from a rhesus macaque monkey placed in a cage in the Ziika Forest of Uganda, near Lake Victoria, by the scientists of the Yellow Fever Research Institute.[78] A second isolation from the mosquito A. africanus followed at the same site in January 1948.[79] When the monkey developed a fever, researchers isolated from its serum a "filterable transmissible agent" which was named Zika in 1948.[80]
First evidence of human infection, 1952[edit]
Zika was first known to infect humans from the results of a serological survey in Uganda, published in 1952.[81] Of 99 human sera tested, 6.1% had neutralizing antibodies. As part of a 1954 outbreak investigation of jaundice suspected to be yellow fever, researchers reported isolation of the virus from a patient,[82] but the pathogen was later shown to be the closely related Spondweni virus.[83] Spondweni was also determined to be the cause of a self-inflicted infection in a researcher reported in 1956.[84]
Spread in equatorial Africa and to Asia, 1951–2016[edit]
Subsequent serological studies in several African and Asian countries indicated the virus had been widespread within human populations in these regions.[80] The first true case of human infection was identified by Simpson in 1964,[85] who was himself infected while isolating the virus from mosquitoes.[80]From then until 2007, there were only 13 further confirmed human cases of Zika infection from Africa and Southeast Asia.[86] A study published in 2017 showed that the Zika virus, despite only a few cases were reported, has been silently circulated in West Africa for the last two decades when blood samples collected between 1992 and 2016 were tested for the ZIKV IgM antibodies.[87]
Micronesia, 2007[edit]
In April 2007, the first outbreak outside of Africa and Asia occurred on the island of Yap in the Federated States of Micronesia, characterized by rash, conjunctivitis, and arthralgia, which was initially thought to be dengue, chikungunya, or Ross River disease.[88] Serum samples from patients in the acute phase of illness contained RNA of Zika. There were 49 confirmed cases, 59 unconfirmed cases, no hospitalizations, and no deaths.[89]
2013–2014[edit]
After October 2013 Oceania’s first outbreak showed an estimated 11% population infected for French Polynesia that also presented with Guillain–Barre syndrome (GBS). The spread of ZIKV continued to New Caledonia, Easter Island, and the Cook Islands and where 1385 cases were confirmed by January 2014. During the same year, Easter Island acknowledged 51 cases. Australia began seeing cases in 2012. Research showed it was brought by travelers returning from Indonesia and other infected countries. New Zealand also experienced infections rate increases through returning foreign travelers. Oceania countries experiencing Zika today are New Caledonia, Vanuatu, Solomon Islands, Marshall Islands, American Samoa, Samoa and Tonga.[90]
Between 2013 and 2014, further epidemics occurred in French Polynesia, Easter Island, the Cook Islands, and New Caledonia.[17]
Americas, 2015–present[edit]
There was an epidemic in 2015 and 2016 in the Americas. The outbreak began in April 2015 in Brazil, and spread to other countries in South America, Central America, North America, and the Caribbean. In January 2016, the WHO said the virus was likely to spread throughout most of the Americas by the end of the year;[91] and in February 2016, the WHO declared the cluster of microcephaly and Guillain–Barré syndrome cases reported in Brazil – strongly suspected to be associated with the Zika outbreak – a Public Health Emergency of International Concern.[4][92][93][94] It was estimated that 1.5 million people were infected by Zika in Brazil,[95] with over 3,500 cases of microcephaly reported between October 2015 and January 2016.[96]
A number of countries issued travel warnings, and the outbreak was expected to significantly impact the tourism industry.[4][97] Several countries have taken the unusual step of advising their citizens to delay pregnancy until more is known about the virus and its impact on fetal development.[15] With the 2016 Summer Olympic Games hosted in Rio de Janeiro, health officials worldwide voiced concerns over a potential crisis, both in Brazil and when international athletes and tourists returned home and possibly would spread the virus. Some researchers speculated that only one or two tourists might be infected during the three-week period, or approximately 3.2 infections per 100,000 tourists.[98] In November 2016, the World Health Organization declared that the Zika virus was no longer a global emergency while noting that the virus still represents "a highly significant and a long-term problem".[99]
As of August 2017 the number of new Zika virus cases in the Americas had fallen dramatically.[100]
The testing market is not expected to take a halt any time soon. Among the major regions of the global market, Latin America was expected to lead with revenue in excess of US$ 2,400 M by the end of 2017. The Caribbean region is anticipated to project the highest growth rate of Zika virus testing market during the forecast period 2017-2020.[101]
Other cases[edit]
On 22 March 2016 Reuters reported that Zika was isolated from a 2014 blood sample of an elderly man in Chittagong in Bangladesh as part of a retrospective study.[102] Zika is also occurring in Tanzania as of 2015/2016.[103]






Comments